Hydroxyapatite (HA)
Hydroxyapatite 3D Printing Materials Introduction
Hydroxyapatite (HA) is a calcium phosphate bioceramic that closely resembles the mineral component of natural bone. It exhibits excellent bioactivity, biocompatibility, and osteoconductivity, making it a prime material for bone tissue engineering and orthopedic implants.
By leveraging advanced ceramic 3D printing, Hydroxyapatite enables custom production of bone scaffolds, dental implants, and porous structures that support bone cell proliferation, integration, and mechanical reinforcement.
Hydroxyapatite Similar Grades Table
Country/Region | Standard | Grade or Designation |
|---|---|---|
USA | ASTM | F1085, F1185 |
ISO | International | ISO 13779-3 |
China | GB | YY/T 0611 |
Japan | JIS | JIS T0330 |
EU | Directive | 93/42/EEC (Medical Use) |
Hydroxyapatite Comprehensive Properties Table
Category | Property | Value |
|---|---|---|
Physical Properties | Density | 3.16 g/cm³ |
Porosity (sintered) | 20–40% | |
Melting Point | ~1500°C | |
Thermal Expansion | 14.8 µm/(m·K) | |
Chemical Composition | Ca/P Ratio | 1.67 |
Calcium Oxide (CaO) | 55–65% | |
Phosphorus Pentoxide (P₂O₅) | 30–40% | |
Mechanical Properties | Compressive Strength (dense) | 100–120 MPa |
Young’s Modulus | 80–110 GPa | |
Hardness | ~500 HV | |
Fracture Toughness | 0.7–1.2 MPa·m½ |
3D Printing Technology of Hydroxyapatite
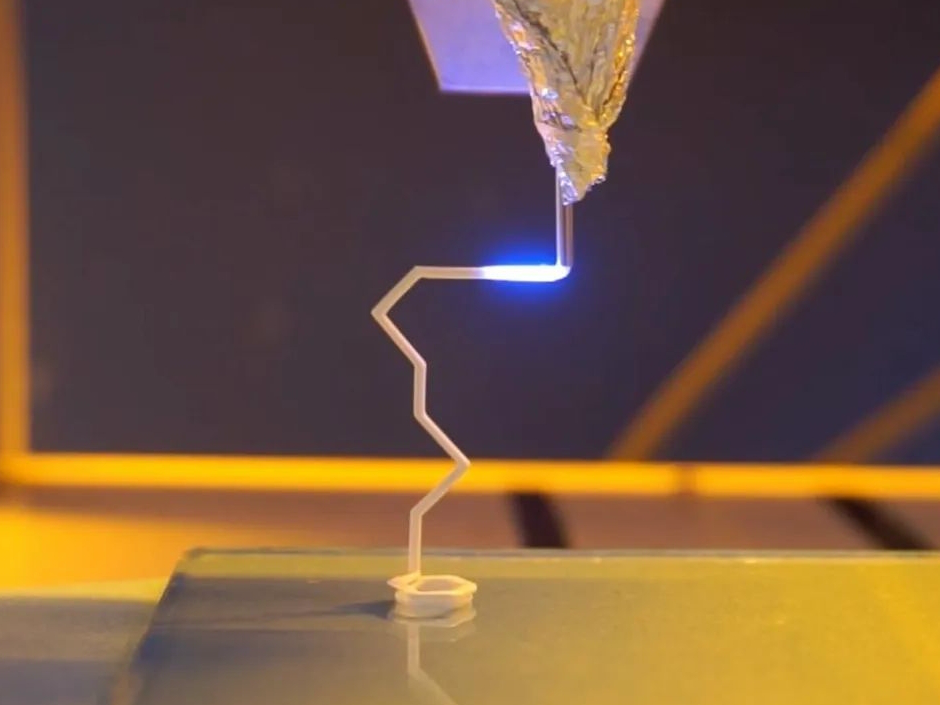
Hydroxyapatite is commonly processed using Vat Photopolymerization (e.g., SLA, DLP), Binder Jetting, and Material Extrusion (e.g., Robocasting). These methods support precise control over geometry and internal porosity, critical for biomedical use.
Applicable Process Table
Technology | Precision | Porosity Control | Suitability |
|---|---|---|---|
SLA/DLP | ±0.05–0.1 mm | Low–Moderate | Dental Implants, Microstructures |
Binder Jetting | ±0.1–0.3 mm | Moderate–High | Bone Scaffolds, Complex Cavities |
Robocasting | ±0.1–0.2 mm | High | Porous Bone Tissue Engineering |
Hydroxyapatite 3D Printing Process Selection Principles
Vat Photopolymerization such as DLP is ideal for achieving fine resolution (±0.05 mm) and smooth surfaces, often used in dental crowns and low-load implants.
Binder Jetting supports moderate resolution (±0.1–0.3 mm) and excellent porosity control, suitable for complex orthopedic implants requiring interconnectivity and load distribution.
Material Extrusion or robocasting offers high porosity (up to 70%) and is favored for patient-specific bone scaffolds that promote osteogenesis and resorption.
Hydroxyapatite 3D Printing Key Challenges and Solutions
Hydroxyapatite is brittle and sintering-sensitive. Cracking and low mechanical strength are common if porosity and particle size are not tightly controlled. Optimizing binder formulation and sintering profiles between 1100–1250°C mitigates internal stress and enhances strength.
High-resolution parts may experience poor layer adhesion due to low ceramic-polymer interaction. Using tailored photo-reactive binders and post-sintering treatments improves cohesion and densification.
Moisture sensitivity during printing must be controlled. Dry powder handling and inert atmospheric sintering (argon or vacuum) prevent hydration and phase changes that compromise biocompatibility.
Typical Post-Processing for Hydroxyapatite 3D Printed Parts
Sintering at 1100–1250°C consolidates the ceramic and increases strength while maintaining controlled porosity for bone integration. Polishing improves surface smoothness for dental or orthopedic use, reducing friction and enhancing biocompatibility. Electropolishing provides fine surface refinement for internal channels and complex geometries in HA components. Surface Coating with biocompatible films enhances osseointegration and corrosion resistance of load-bearing implants.
Industry Application Scenarios and Cases
Hydroxyapatite 3D printing is widely used in:
Medical and Healthcare: Custom bone grafts, maxillofacial implants, and porous scaffolds for orthopedic surgery.
Dental: Crowns, bridges, and root analogs that support cell growth and biointegration.
Biotech Research: In vitro bone models, regenerative medicine platforms, and drug delivery structures.
One case study involved printing custom porous scaffolds for craniofacial reconstruction using DLP-based HA printing, achieving >98% bone ingrowth after 12 weeks in vivo with excellent dimensional matching and biocompatibility.
FAQs
What are the primary applications of 3D printed Hydroxyapatite in medical fields?
Which 3D printing method offers the best resolution for Hydroxyapatite parts?
How does Hydroxyapatite compare with other bio-ceramic materials in 3D printing?
What are the key challenges in Hydroxyapatite 3D printing, and how are they resolved?
Can Hydroxyapatite scaffolds be customized for patient-specific bone structures?