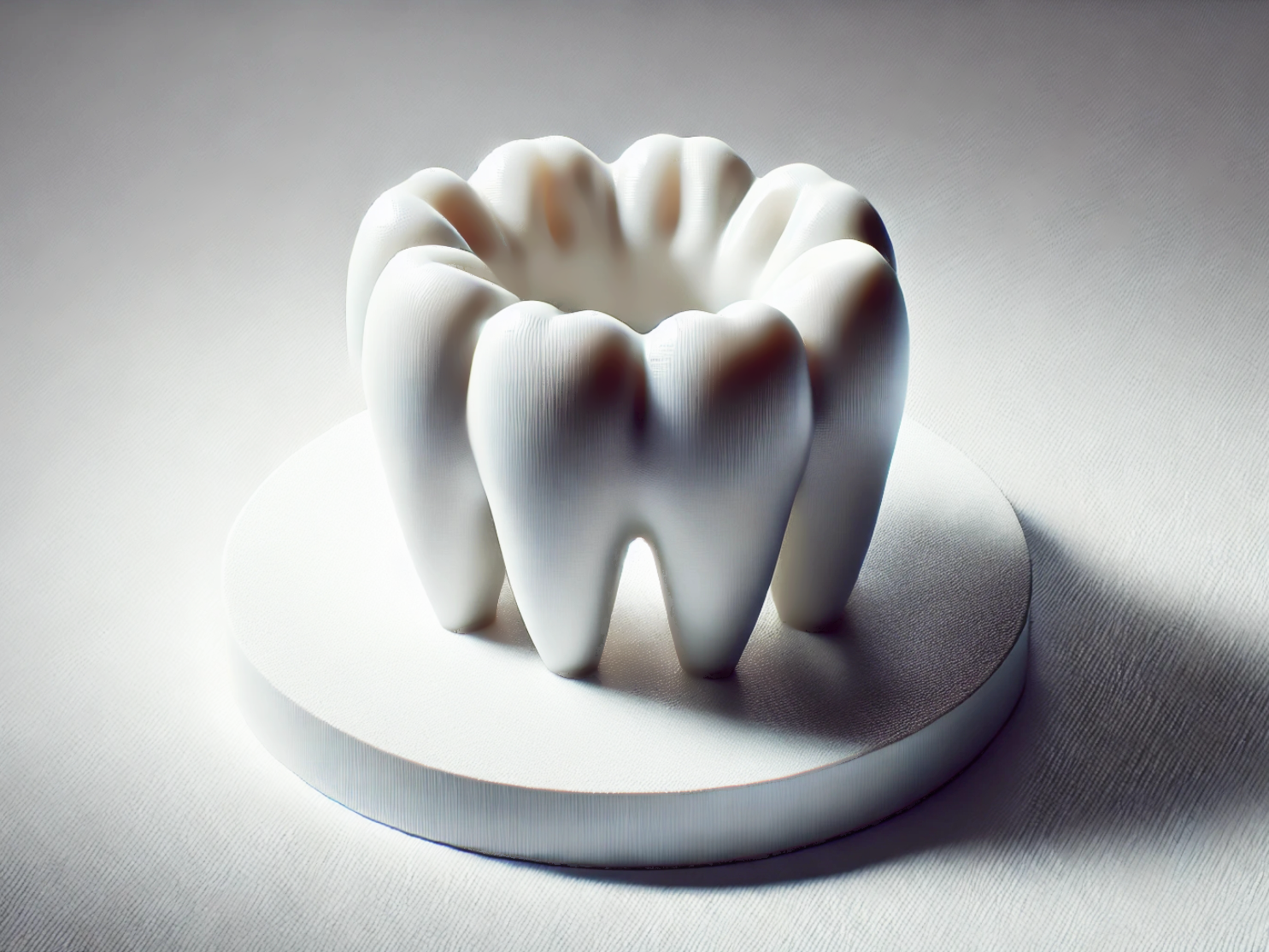
Zirconia (ZrO2) 3D Printing: Precision 3D Printed Dental Tooth Implants
Introduction
Zirconia (ZrO₂) 3D printing has become a breakthrough technology in the dental field, producing high-precision, durable, and biocompatible dental tooth implants. Utilizing ceramic 3D printing technologies such as Vat Photopolymerization and Material Extrusion, Zirconia (ZrO₂) dental components achieve excellent mechanical strength, aesthetics, and long-term stability.
Compared to conventional milling methods, Zirconia 3D printing shortens lead times, reduces material waste, and enables patient-specific, highly complex implant designs with minimal post-processing.
Applicable Material Matrix
Material | Purity (%) | Flexural Strength (MPa) | Hardness (HV10) | Fracture Toughness (MPa·m¹/²) | Translucency (%) |
|---|---|---|---|---|---|
>99% | 900–1200 | 1200–1400 | 6–10 | Medium | |
>99% | 700–900 | 1000–1200 | 3–6 | High | |
>99% | 850–1000 | 1100–1300 | 5–7 | Medium-High |
Material Selection Guide
3Y-TZP Zirconia (3 mol% Yttria-Stabilized): Excellent for root-form dental implants due to its superior strength, fracture toughness, and aging resistance.
5Y-PSZ Zirconia (5 mol% Yttria-Stabilized Partially Stabilized): Ideal for anterior restorations requiring high translucency and aesthetic appearance.
4Y-PSZ Zirconia: Suitable for bridge frameworks and posterior implants, balancing strength and translucency.
Process Performance Matrix
Attribute | Ceramic 3D Printing Performance |
|---|---|
Dimensional Accuracy | ±0.05 mm |
Density (after sintering) | >99% Theoretical Density |
Minimum Wall Thickness | 0.5 mm |
Surface Roughness (As-Sintered) | Ra 2–5 μm |
Feature Size Resolution | 100–150 μm |
Process Selection Guide
Superior Strength and Durability: Zirconia implants deliver flexural strengths up to 1200 MPa, outperforming traditional dental ceramics in mechanical performance.
Biocompatibility: In the human body, zirconia exhibits excellent tissue integration, low bacterial adhesion, and minimal allergic reactions.
High Aesthetic Quality: The natural white color and optional translucency of zirconia provide outstanding visual outcomes for visible dental restorations.
Precision Fit: 3D printing enables highly accurate, patient-specific geometries directly from intraoral scans, reducing clinical adjustment time.
Case In-Depth Analysis: Customized 3Y-TZP Zirconia Dental Implants
A dental clinic required customized root-form implants offering exceptional mechanical properties and patient-specific anatomical matching. Our Zirconia 3D printing service with 3Y-TZP material produced implants, achieving flexural strength above 1100 MPa, dimensional accuracy of ±0.05 mm, and over 99% theoretical density after sintering. In clinical follow-up evaluations, the implants showed perfect primary stability during insertion and excellent osseointegration. Post-processing included polishing and CNC machining for precise thread structures.
Industry Applications
Dental and Maxillofacial
Patient-specific dental root implants.
Customized crowns, bridges, and veneers.
Full-arch zirconia-supported restorations.
Medical and Healthcare
Maxillofacial implants and bone replacement scaffolds.
Orthopedic spacers and small joint replacements.
Customized craniofacial reconstruction components.
Prosthodontics
Aesthetic anterior crowns with high translucency.
Zirconia abutments for implant-supported dentures.
Temporary and permanent dental prosthetics.
Mainstream 3D Printing Technology Types for Zirconia Dental Components
Vat Photopolymerization (SLA/DLP): Preferred for high-resolution, fine-detail zirconia parts requiring excellent surface finish.
Material Extrusion: Effective for larger dental frameworks with high density after sintering.
Binder Jetting: Useful for batch production of dental zirconia components requiring cost-effective scaling.
FAQs
What types of Zirconia materials are best for dental 3D printed implants?
How does Zirconia 3D printing compare to traditional milling for dental applications?
What post-processing techniques are used for 3D printed Zirconia implants?
Can 3D printed Zirconia achieve sufficient translucency for aesthetic dental restorations?
How accurate are 3D printed Zirconia dental parts compared to conventional manufacturing methods?